A troubling new study published in the Lancet journal eClinical Medicine reveals that women who receive genetic testing and discover they carry a BRCA gene mutation outside of a clinical setting may be making major, life-altering health decisions based on an overestimation of their actual lifetime breast cancer risk.
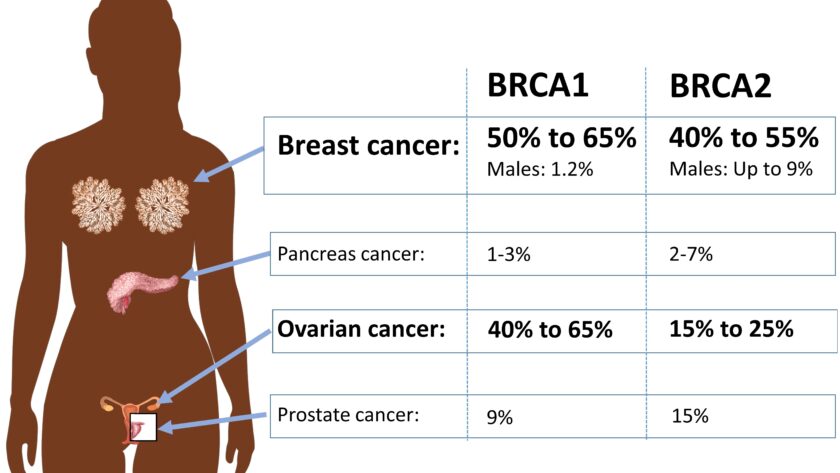
BRCA1 and BRCA2 are tumor suppressor genes. Harmful mutations in these genes can significantly increase a woman’s risk of developing breast and ovarian cancer. However, the level of risk depends heavily on family history and other clinical factors.
The study found that simply having a pathogenic BRCA mutation only elevated breast cancer risk to 18-23% by age 60. But women who learn their BRCA status through direct-to-consumer genetic testing kits or participation in genetic research are often told their lifetime breast cancer risk is a frightening 60-80%.
This inflated, blanket risk estimate could lead some women to undergo unnecessary, invasive preventive mastectomies or oophorectomies that they may later regret.
“Being told you are at high genetic risk of disease can really influence levels of fear of a particular condition and the resulting action you may take,” said lead author Dr. Leigh Jackson of the University of Exeter Medical School. “Up to 80% lifetime risk of developing breast cancer sounds incredibly high compared to a more moderate risk of 20% by age 60. That difference in risk perception could well influence someone’s decision to undergo risky and irreversible surgery like preventive mastectomy.”
How BRCA Risk Estimates Became Skewed Over Time
In the past, full sequencing of the BRCA genes was only offered to women who had already been diagnosed with breast or ovarian cancer at a young age or had multiple close relatives with these cancers. Understandably, these women were already at the highest risk end of the spectrum.
The initial BRCA risk estimates were calculated based on breast and ovarian cancer rates within these families with extensive cancer histories. The estimates did not account for women with BRCA mutations and no family history of breast cancer.
Today, BRCA testing is readily available to any curious consumer via companies like 23andMe without any vetting of personal or family health history. Participants in genetic research studies also often receive results related to cancer risks as an ancillary finding, regardless of their cancer family history. However, the dated, blanket 60-80% lifetime breast cancer risk statistic still pervades consumer test reports and genetic counseling sessions.
“We’d urge that anyone communicating cancer risk does so based on a detailed family history, not just genetics alone,” stressed Dr. Jackson.
Re-Evaluating True BRCA Breast Cancer Risk in the General Population
To determine a more accurate, nuanced picture of BRCA-related breast cancer risk, Dr. Jackson and colleagues analyzed health data on over 450,000 middle-aged UK Biobank research participants. Notably, only 3% of women enrolled had a first-degree relative with breast cancer.
Among women with a BRCA2 mutation, breast cancer risk by age 60 was just 18% for those without a family history of the disease. Even for those with a family history, the risk only increased to 24% by age 60. For the BRCA1 gene, risks were 23% and 45% respectively. While elevated, these risk estimates are clearly far lower than the 60-80% lifetime risk figure commonly quoted.
“Being told you are at high genetic risk of disease can really influence levels of fear of a particular condition and the resulting action you may take,” reiterated Dr. Jackson. “For a woman without a significant family history of breast cancer, a risk of just 18-23% by age 60 may not warrant such aggressive measures as preventive bilateral mastectomy.”
This nuanced understanding of BRCA risk based on family history as well as gene status is crucial for women making major medical decisions like mastectomy.
Overestimating Genetic Risks of Other Hereditary Cancers
Beyond BRCA mutations, the Exeter researchers also looked at risk estimates for Lynch syndrome, a hereditary condition that increases colon cancer risk. Again, they found risks were vastly overstated if not considering detailed family history.
Study co-author Professor Caroline Wright warns that overestimating disease risks could have serious ramifications across the board as direct-to-consumer genetic testing and predisposition research screening become more common.
“We need to ensure we are carrying out rigorous research to find the true risk levels for genetic variants in the general population,” said Wright. “We also must be responsible in how we communicate risk to consumers, to avoid unnecessary fear and distress which may motivate major, potentially harmful medical decisions.”
Rethinking the Need for Aggressive Early Prevention Measures
Learning one’s BRCA mutation status often prompts major preventive health decisions like risk-reducing mastectomy or oophorectomy before cancer can develop. However, the study authors strongly caution against rushing into aggressive measures based on BRCA gene status alone, without a complete understanding of one’s individual risk based on family history and other clinical factors.
“Some women may decide to go ahead with preventive mastectomy or oophorectomy knowing that the risk is 20%, but we want them to make a fully informed decision,” emphasized Dr. Jackson. “We’d urge that anyone communicating cancer risk does so based on a detailed family history, not just genetics alone.”
Likewise, overestimating Lynch syndrome risk due to genetic testing could lead some patients to undergo unnecessary, frequent colonoscopies starting at a young age or even pursue preventive colectomies unlikely to provide benefit.
Prudent Steps if You Have a Concerning Genetic Test Result
If you discover you have a potentially dangerous BRCA mutation or other genetic red flag outside of a clinical setting, first have an in-depth discussion with your doctor before taking any major action. Share your detailed family health history and any risk estimates you were given by the testing company.
Ask your doctor to help objectively contextualize what your test result means for your personal cancer risk based on your unique family background. Together, you can decide if more intensive screening measures or even preventive surgeries are truly warranted in your case.
Stay up-to-date on the latest genetic risk research related to your particular mutation as well. Risk estimates for some genetic variants are likely to change over time as we collect more population data beyond high-risk groups.
Adding Preventative Foods & Drinks Into Your Diet Can Greatly Reduce Your Risk Of Developing Cancer, & Has Even Been Shown To Shrink Already Existing Tumors. I Highly Recommend Checking Out Starwest Botanicals Essiac Tea, & Drinking 1-2 Cups Every Day.
Click Here To Learn More About
Starwest Botanicals Essiac Tea
The Takeaway
At-home genetic testing provides intriguing, personalized health insights for consumers. But disease risk estimates for concerning hereditary mutations are often over-inflated when not considering the full clinical context.
Before making major, irreversible medical decisions based on genetic test results alone, have an in-depth discussion with your doctor to understand your personal risk. Rushing into aggressive treatments without a thorough understanding of your actual risk in context can lead to unnecessary stress and physical harm.
When it comes to genetic disease risks, information and interpretation are powerful. Make sure you have all the facts around your unique risk factors before taking action. Your health deserves nothing less.